Ppo Providers Are Paid Based on Which of the Following
You pay less if you use providers that belong to the plans network. Like an HMO you pay no deductible and usually only a minimal co-payment when you use a healthcare provider within your network.
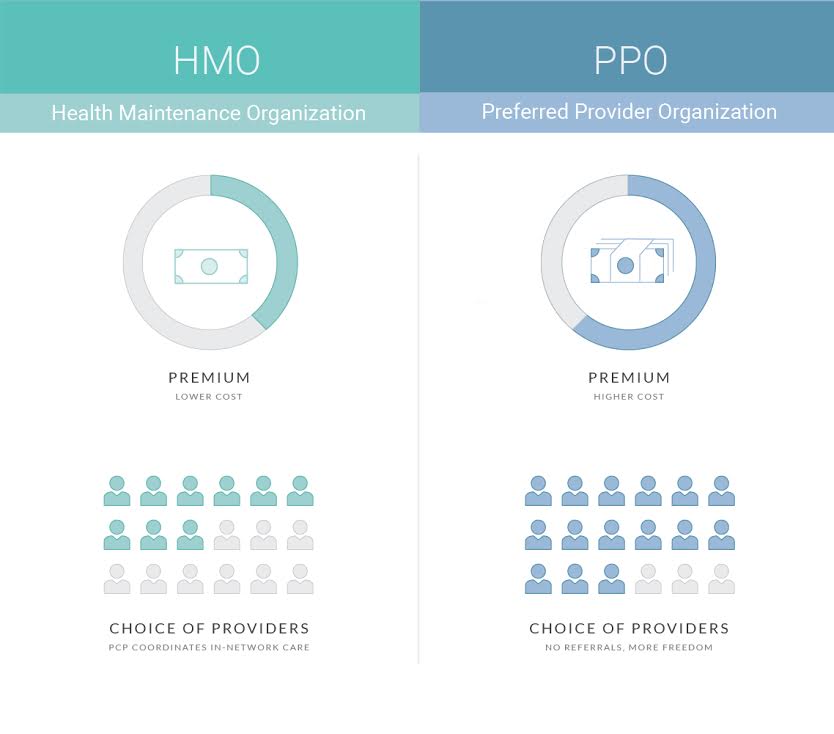
Hmo Vs Ppo What S The Difference
BCBSM will determine Providers payment rate based on documentation of Providers Medicare RHC per-visit rate namely Providers most recently received RHC per-visit rate letter from CMS.

. 12 For PPO Network Providers you pa y the f ollo wing por tion based on the Allowed Amount. Lower Premium Higher Out-of-Pocket. PPO Plans have network doctors other health care providers and hospitals.
Both kinds of help are based on your annual household income and family size. Cost you pay every month for health care coverage. A Medicare PPO Plan is a type of Medicare Advantage Plan Part C offered by a private insurance company.
An HMO is paid a monthly premium for ongoing services while a PPO collects no money until after services are rendered. An HMO requires the insured individual to go to a provider within their. Like virtually all types of health coverage a PPO uses cost-sharing to help keep costs in check.
Unit 2 Discussion 1. The carriers Fee Schedules. Think higher cost with greater flexibility.
Preferred Provider Organization PPO the deepest discount network Premier Network Delta Dentals broader network including most local providers Out-of Network Lowest coverage levels. While HMO and PPO plans are the 2 most common plans especially when it comes to employer-provided health insurance there are other plan types you should know about including EPO and POS plans. A Non-PPO Network or a Non-Contracting Provider you pay the following portion based on the applicable Allowed Amount or Non-Contracting Amount 2 For Covered Services received from a PPO Network Provider you pay the f ollowing por tion based on.
Cost-sharing reductions available on Enhanced Silver plans lower what you pay for services like doctor visits. For Contracting Non-PPO Network Providers you pay the following portion based on the Allowed Amount. Set up an insurance plan with a PPO Percentage plan type and the carrier fee schedule.
You can also use outofnetwork providers for. PPO plans also assimilated the. Set up a PPO plan and track write-offs.
You can use doctors hospitals and providers outside of the network for an additional cost. Review managed care contracts for different payment plans PPO HMO Fee for services etc and describe provider incentives and risks under each of the following reimbursement methods. When you see the healthcare provider or use healthcare services you pay for part of the cost of those services yourself in the form of deductibles coinsurance and copayments.
They may seek the services of any licensed provider anywhere in the US. But the employers that are paying for the provider-network-based coverage now face a similar lack of information about the operations of the provider networks. Other types of health plans.
PPO benefits are based upon a three-tier network. A Non-PPO Network or a Non-Contracting Provider you pay the following portion based on the applicable Allowed Amount or Non-Contracting Amount 2 For Covered Services received from a PPO Network Provider you pay the f ollowing por tion based on the Allowed Amount TYPE OF SERVICE Institutional and Professional. On the in-network side of the plan a participant who uses their primary care physician visits a specialist has an emergency room or urgent care visit andor uses the prescription program will incur a fixed dollar copay for each visit.
Cost-based Cost-based reimbursement is one of the most common methods of payments in health insurance. PPO patients are not limited to only those providers in the PPOs network. Hospitals are paid using the Medicare Prospective Payment System.
All out-of-network MA claims go through the same. PPO members are not covered for service provided out of network. The USA Care PPO plan reimburses Medicare providers at the Medicare rate minus any member co-payments or co-insurance for medically necessary services covered by the plan.
Insurance estimates will be based on the carriers fee schedule. All network PPO hospitals and ambulatory surgical centers ASCs were evaluated and assigned to one of two in-network benefit tiers based on cost and minimum quality standards. Hospital outpatient departments.
PPOs operate on a fee-for-service basis. However it may be necessary for a procedure to be _________________ before a claim will be paid it does not matter where the procedure is performed. Services for urgent or emergency care are paid based on in-network benefits.
POS plans A Point of Service POS plan is a type of managed healthcare system that combines characteristics of the HMO and the PPO. For an inpatient or outpatient procedure or for most medical services on the out-of-network. Physicians and other health professionals are paid based on the Medicare Fee Schedule.
BCBSM will pay Provider one hundred one percent 101 of the above-referenced Medicare RHC per-visit rate less the applicable patient co-. Premium assistance is available if you qualify for all plans except Minimum Coverage plans. PPO members only pay a fixed copay for each service received.
For Non-Contracting Providers you pay the following portion based on the Non-Contracting Amount and may be balance billed. An HMO allows the insured individual to choose from a list of providers while a PPO assigns the insured individual the provider nearest his or her residence. A contracted MA PPO provider.
Tier 2 members pay a higher cost-sharing for hospital and outpatient surgery services when. The PPO pays part. You pay less if you use doctors hospitals and other health care providers that belong to the plans network.
Preferred Provider Organization PPO A type of health plan that contracts with medical providers such as hospitals and doctors to create a network of participating providers. On the Insurance Plan select these options. Gapenski and Reiter 2012 state.
Type of plan and provider network. This plan tracks write-offs. Providers are paid up to reasonable and customary rates.
Benefits will be based on the Medicare allowed amount for Medicare covered services based on where services are rendered and paid under the members out-of-network benefits. PPO providers are paid a modified fee for service basis a They agree to provide services at a discount from full charge b They agree to not balance bill the patient eg. Tier 1 members pay the lowest cost-sharing for hospital and outpatient surgery services.
A PPO plan is also generally more expensive than an HMO plan. Normal Charge for a procedure 100 Preferred Provider agree to discount 75 Copayment 5 PPO Payment 70 c Providers in PPOs are not at financial risk for over-utilization. How PPO Plans Work.
PPOs typically require primary physicians referral to a specialist.

24 Total Compensation Statement Excel Template Statement Template Employee Benefit Excel Templates

How Do Commerical Ppo Vs Hmo Insurance Plans Work Dr Wenjay Sung Podiatrist

No comments for "Ppo Providers Are Paid Based on Which of the Following"
Post a Comment